Hospitals in Vietnam are continuously introducing the latest technological advancements and improvements to their operating theaters, opening up limitless options for patients with previously inoperable conditions.
H.B. from Long Bien District, Hanoi found herself faced with impaired vision in one eye and complete loss of eyesight in the other at the age of 37.
Magnetic resonance imaging (MRI) scan results indicated the growth of a pituitary tumor inside her skull which was interfering with her ability to see.
B. received surgery at Viet Duc University Hospital (VDUH), a central-level medical facility in the capital city, where the surgeons employed a novel technique to remove the three-centimeter-large tumor through her nasal cavity.
She gained back a portion of her eyesight within 24 hours of the operation and a majority of her sight in just five days. She was discharged from the hospital on the sixth day.
“I’ve gained more vision and a larger visual field each day since the discharge. It has almost returned to normal,” B. said.
The technique was done by inserting medical instruments through the nostrils, then incising parts of the sphenoid sinus — a hollow space in the skull behind the nasal passages and below the brain — to create an opening to the tumor, utilizing the navigation system to locate the mass, cutting the growth into pieces, and finally removing it through the nasal passage, Dr. Nguyen Thanh Xuan, deputy head of the VDUH's neurosurgery department 1, explained.
This technique – called transsphenoidal surgery – is used to remove pituitary tumors, meningeal tumors, and craniopharyngioma, a rare type of brain tumor.
The oral passage, which is also a natural orifice, can be used to remove tumors placed lower in the skull, such as in the basilar area.
The unconventional placement of the laceration requires special materials to help heal the surgical wound, such as nasal mucosa to leg fat.
“The application of such materials on an open wound helps the body to fully mend in just a few days. That’s how magnificent our bodies are,” Xuan said.
|
|
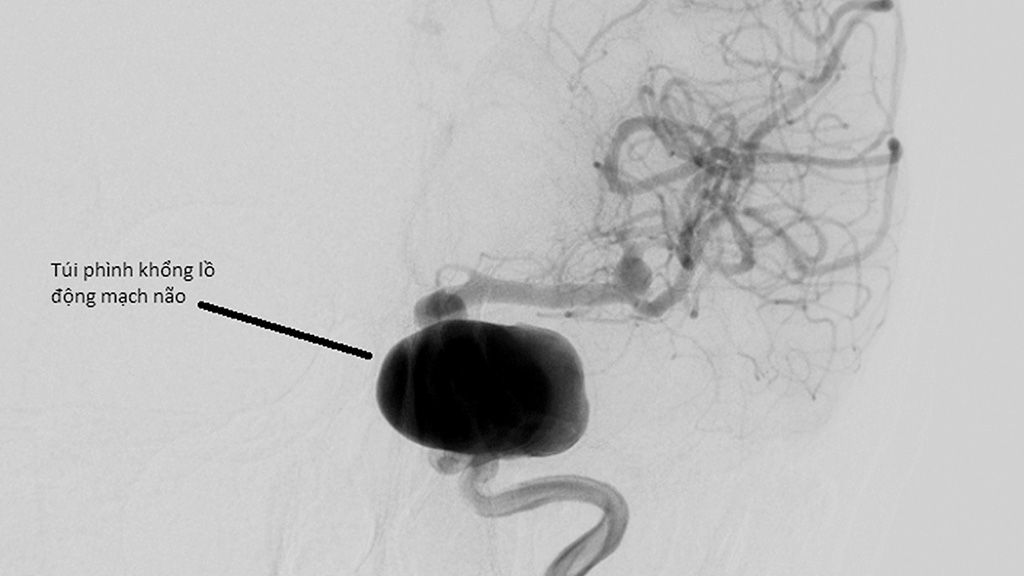
| An aneurysm balloon in a brain artery is shown in a supplied file photo achieved through medical imaging. |
In his younger days, Xuan would not have dreamt of a surgical method that allows alterations to be done through nasal and oral passages.
But modern techniques have surpassed his wildest expectations, bringing about cutting-edge treatment approaches with certified effectiveness, given medical advances and equipment utilization.
Compared to conventional open surgeries, natural orifice endoscopic methods do not inquire the brain to be uncovered, minimalizing the risk of brain impact and the size of incisions while allowing the wound to heal faster.
This is considered a medical breakthrough as it can be used on 90 percent of pituitary tumor cases, helping patients access a significantly better surgical experience.
However, according to Xuan, not many surgeons are capable of performing this method as it requires expertise in endoscopic surgery, microsurgery, and many other advanced techniques that can only be made possible with the support of the latest technological instruments.
Wide awake while being cut open
Experiencing brain surgery without being put to sleep, also called awake craniotomy, is a new approach that has been applied on several recent patients at the VDUH.
C.Q.C., a 56-year-old from the north-central province of Quang Binh, is one of them.
C. was experiencing numbness in his left hand, movement limitations, an inability to grab objects, and the occasional loss of balance while walking before he sought treatment.
At the VDUH, practitioners found a large tumor — 2.3 centimeters in width and 3.6 centimeters in length — in C.’s brain and suggested removing it using the awake craniotomy technique, to which C. agreed.
During the three-hour surgery, C. was kept awake in the first two hours and was even able to talk and sing when asked in order to signify his response to the surgeon’s intervention and help doctors monitor whether his language or motor nerves were obstructed.
Contrary to an assumed panic response, C. coped quite well with being awake during the surgery and even said that being able to interact with doctors during the procedure was quite exciting.
After the surgery, the patient said he was able to wiggle the fingers in his left hand and that he had gained back the ability to use chopsticks.
Dr. Dong Van He, deputy director of the VDUH, an adept surgeon in awake craniotomy, talked of the method as a newly introduced option, one that inquires the courage of the patients to endure the sound of surgical drills and blades cutting into their own skull.
|
|
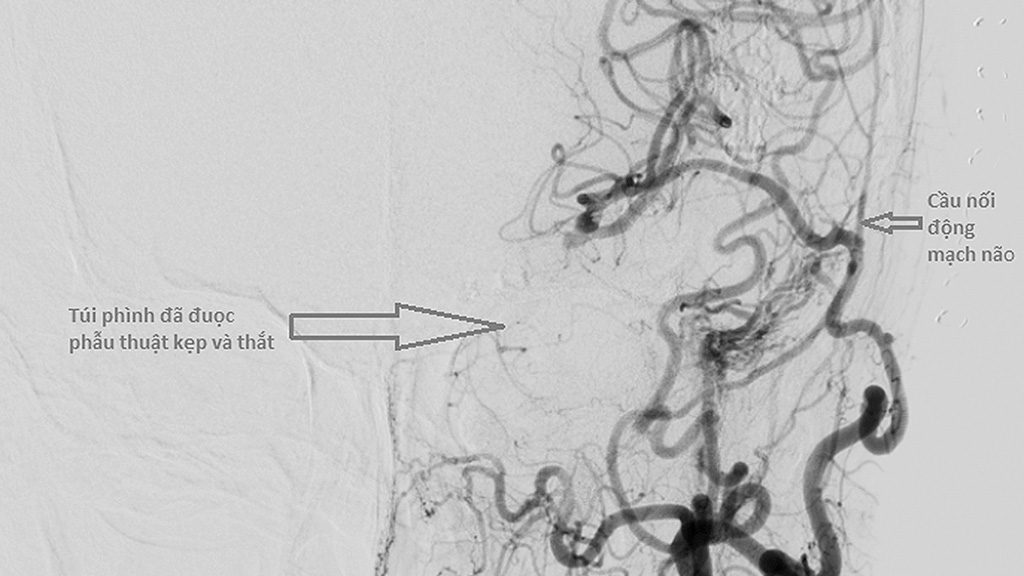
| Blood vessels are inserted and an aneurysm balloon is nullified using the artery bypass technique in a supplied file photo of the brain achieved through medical imaging. |
Artery bypass
Dr. Ngo Manh Hung, deputy head of the VDUH's neurosurgery department 1, said an artery bypass is a procedure that can be indicated to cases of brain aneurysm or clogged brain arteries, which inherently come with risks of stroke.
Doctors in the past mostly resorted to two kinds of intervention — removing the aneurysm and reconnecting the severed ends of the blood vessels or blocking the blood flow from the dilated section of the artery.
These methods had not proven to be effective when it comes to cases of multiple or oversized aneurysms, which gave rise to a demand for alternative approaches capable of nullifying aneurysm balloons and preserving the arteries.
“In those cases, we perform artery bypasses because they work both as a medically-approved response and as a financially viable alternative to traditional disciplines which can cost hundreds of millions of Vietnamese dong [VND100 million = US$4,300],” Hung said.
Artery bypasses are also employed in cases of progressing brain ischemia — insufficient blood flow to the brain — and narrowing brain arteries which predispose patients to the risk of stroke, health decline, paralysis, memory decline, and epilepsy, but less frequently compared to brain aneurysms, according to Hung.
The technique also resolves conditions where artery tapers, triggering the body to generate a new passage for blood to reach the brain.
It is a disease which bears a resemblance to progressive brain ischemia in terms of its mechanisms and is gradually being given more public awareness.
The circumstantial artery created by the body is weak and susceptible to bursts. The consequences are divided into two scenarios.
One of these scenarios is prevalent in children since their growing brain demands larger amounts of blood. which triggers the human body to create more makeshift arteries and in turn multiplies the risk of bursting.
The other is seen among elders and involves the main artery failing, putting pressure on the new arteries, which leads to eventual bursts. Artery bypasses would address this situation as it helps with supplying enough blood to the brain.
|
|
| Dr. Ngo Manh Hung, deputy head of the neurosurgery department 1 under Viet Duc University Hospital in Hanoi, Vietnam, explains the artery bypass technique in brain surgery with hand-drawn visualization. Photo: L. Anh / Tuoi Tre |
“The artery bypass technique has been done at the VDUH for many years, the only difference being that facilities in the past were undersupplied, with sutures not enough to do the standard regimen. For the moment, we are practicing it while much better equipped,” Hung revealed.
The technique requires coordination between multiple surgeons, including vascular and neural specialists, in two phases.
In the first phase, the vascular surgeon takes a blood vessel from the leg and passes it to the neurosurgeon to be rerouted from the neck to arteries in the brain.
The other phase entails retrieving blood vessels from the scalp and inserting them into the arteries in the brain. The vessels are as small as one millimeter in diameter and must be joined using minuscule sutures.
Just a few years ago, the medical sector was not in favor of artery bypasses and instead embraced the method of coronary intervention until they realized the high relapse rate of the latter and gradually switched to the former.
Brain intervention used to be stigmatized by patients as a hazard to memory and life quality. But Dr. Hung claimed: “Artery bypasses do not affect memory since the process requires us to ‘lock’ blood flow inside the artery wall.”
“It took us 13 minutes with 12-14 sutures to attach [a pair of] arteries’ loose ends, which means roughly one minute for a suture. This is close to the international standard, which is around 15 minutes,” Hung said.
“My teacher in Japan can do it in 11 minutes. […] Theoretically speaking, the faster it takes, the quicker we can reintroduce blood flow into the arteries, which means fewer complications are likely to arise.”
Like us on Facebook or follow us on Twitter to get the latest news about Vietnam!